Lede
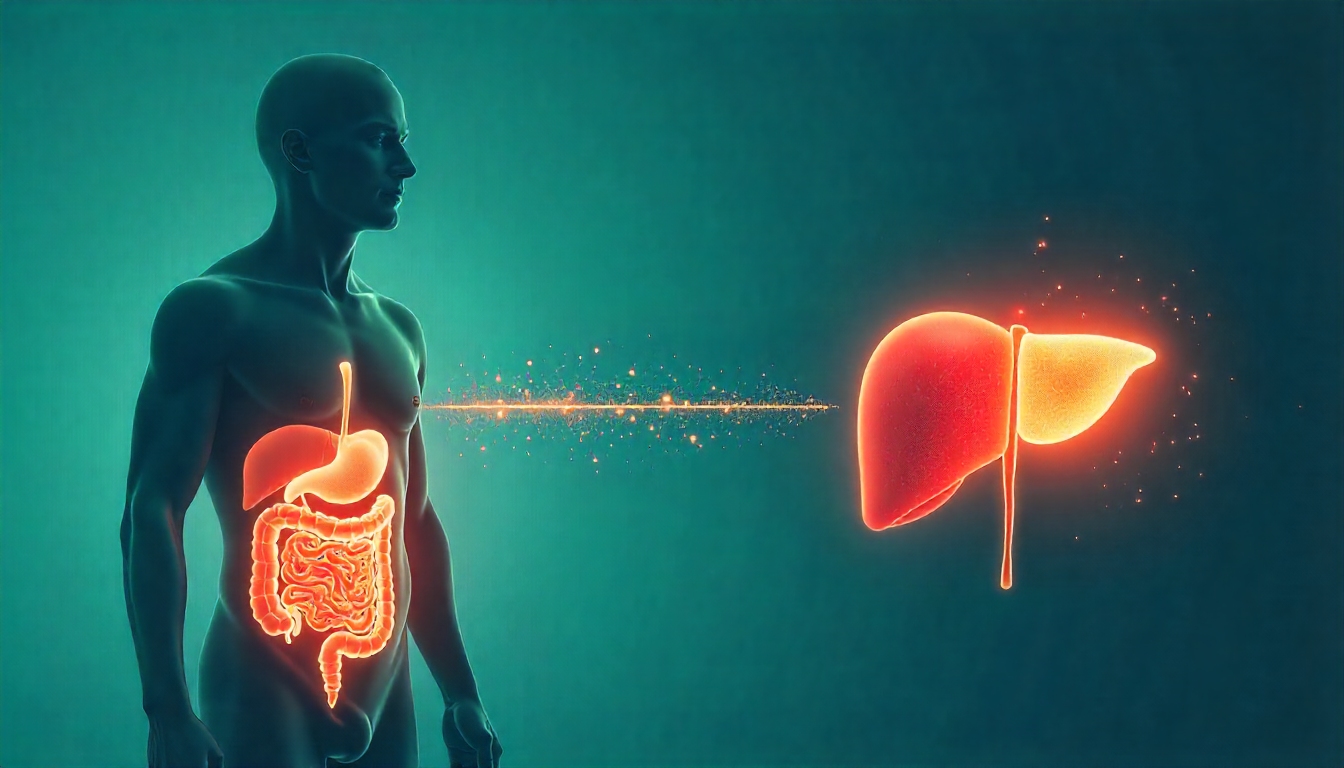
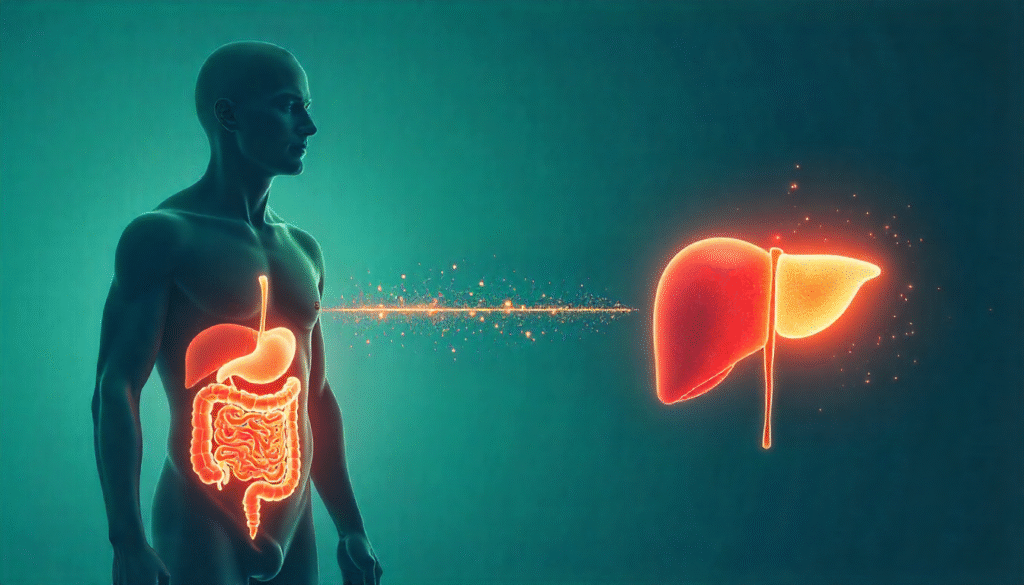
A Canadian research team has identified a gut-derived metabolite — D-lactate — that can enter the bloodstream and prompt the liver to produce excess sugar and fat. The discovery, published in Cell Metabolism, points to a new, microbiome-centered approach to prevent or treat metabolic dysfunction-associated steatotic liver disease (MASLD). PubMed+1
What the study shows
Researchers found that D-lactate produced by gut microbes can bypass known metabolic checks and directly fuel hepatic glucose and lipid synthesis. In obese mouse models, trapping the bacterial D-lactate in the gut improved blood sugar, insulin resistance and markers of liver inflammation and fibrosis — without changing diet or body weight. These findings imply that blocking the microbial signal before it reaches the liver may reduce metabolic damage. PubMed+1
Expert view and mechanism
Professor Jonathan Schertzer of McMaster University and collaborators describe this as a previously unrecognized branch of host-microbial metabolism: historically, lactate exchange was considered mainly between muscle and liver; the study extends that axis to include the microbiome. That insight reframes how clinicians and researchers might target fatty liver and related metabolic diseases. Brighter World+1
Why this matters clinically
MASLD — formerly called non-alcoholic fatty liver disease (NAFLD) — affects a large share of the population and is strongly linked to obesity and type 2 diabetes. If left untreated it can progress to inflammation, fibrosis, cirrhosis and liver cancer. Targeting a microbial metabolite that directly drives hepatic sugar and fat production opens a new therapeutic avenue that could complement weight-loss strategies and glycemic control. British Liver Trust+1
Public-health context (UK)
Fatty liver disease is estimated to affect up to 1 in 5 people in the UK, and nearly two-thirds of adults in England are overweight or living with obesity — key drivers of MASLD. The rising prevalence of obesity has increased urgency for preventative and treatment options at scale. British Liver Trust+1
Interplay with current obesity treatments
Rapid uptake of GLP-1/tirzepatide-class weight-loss medications has changed the obesity-care landscape. Industry and market data estimate roughly 1.5 million people in the UK were using weight-loss medications (including privately procured injections) in early 2025 — showing both the scale of demand and the need for complementary interventions that directly protect the liver. Microbiome-targeted therapies could be an important adjunct for patients who remain at risk of MASLD despite weight loss. The Pharmacist+1
Next steps and research priorities
The study’s promising preclinical results now require: (1) validation in larger and more diverse human cohorts, (2) identification of the specific bacteria responsible and the molecular pathways involved, and (3) development of safe, gut-targeted agents (for example polymers or oral traps) that can neutralize D-lactate or alter its production. Clinical trials will be needed to confirm efficacy and safety in people. PubMed+1
Takeaway
This discovery strengthens the case for viewing the gut microbiome as an active metabolic organ that can drive liver disease. Blocking microbial D-lactate before it reaches the liver could become a novel, complementary strategy in the fight against MASLD — potentially reducing progression to severe liver damage while other metabolic treatments (diet, GLP-1s, diabetes drugs) are optimized. PubMed+1
Further reading / sources (add these as external links on your article)
- Cell Metabolism — PubMed / journal entry for the paper (Fang H. et al., Cell Metabolism). PubMed
- McMaster University news: “Trapping gut bacteria’s hidden fuel improves blood sugar and liver health”.